Lab and venue hygiene best practices
Our Coffee Quality Institute team was asked to develop best practices enabling attendees to feel confident in the sanitation procedures of our venues.
The official CQI release is linked here
Full text below:
The purpose of this document is to assist Q Instructors and Assistant Instructors in helping the labs and venues in which they operate utilize current cleaning and disinfecting best practices. The more aware potential course attendees are regarding the hygiene practices of a facility, the more likely they are to feel confident and safe engaging the services of that facility. The sooner we can get back into the teaching labs and venues the better!
According to the Center for Infectious Disease Research and Policy (CIDRAP) the COVID-19 outbreak will not end until 60% to 70% of the human population is immune to the virus, which may take between 18 and 24 months. According to the Center for Disease Control a vaccine may not be publicly available until Q1, 2021. Because of this, new sanitation standard operating procedures for labs and venues are required.
At the end of this document you will find a High-Touch Point Cleaning Checklist and links to infographics, many of which are available in multiple languages. Please use these tools and recommendations to assist the labs and venues.
Know the difference between Cleaning, Disinfecting and Sanitizing
One of the most effective things that you can do to promote safety in the minds of potential lab and venue attendees is to make your procedures for cleaning, disinfecting, and sanitizing known.
Cleaning removes germs, dirt, and impurities from surfaces or objects. Cleaning works by using soap or detergent and water to physically remove germs from surfaces. This process does not necessarily kill germs, but by removing them, it lowers their numbers and the risk of spreading infection.
Disinfecting kills germs on surfaces or objects. Disinfecting works by using chemicals to kill germs on surfaces or objects. This process does not necessarily clean dirty surfaces or remove germs, but by killing germs on a surface after cleaning, it can further lower the risk of spreading infection.
Sanitizing lowers the number of germs on surfaces or objects to a safe level, as judged by public health standards or requirements. This process works by either cleaning or disinfecting surfaces or objects to lower the risk of spreading infection.
Definitions courtesy of the US Center for Disease Control.
Clean and Disinfect surfaces that are touched often
One of the most effective things that you can do to reduce the risk of spreading a virus or bacteria and lower the number of germs in a lab and venue is to sanitize the High-Touch points.
Most studies have shown that the flu virus can live and potentially infect a person for up to 48 hours after being deposited on a surface. According to the New England Journal of Medicine, COVID 19 has a variable length of contagion on a surface:
- Glass = 5 Days
- Wood = 4 Days
- Plastic = 3 Days
- Stainless Steel = 3 Days
- Cardboard = 24 Hours
- Copper = 4 Hours
We have created a High-Touch Point checklist that is representative, but not exhaustive, for identifying commonly touched places in a lab and venue. We suggest that you use this checklist as a guide and walk through the facility thoughtfully considering what an attendee might likely touch often and what might logically be touched by multiple attendees.
See High-Tough Checklist linked here.
Perform regular and routine cleaning and disinfecting
One of the most effective things that you can do to reduce the potential presence of a virus or bacteria is regular routine cleaning and disinfecting.
Fortunately, flu viruses are relatively fragile, so standard cleaning and disinfecting practices are sufficient to remove or kill them. Follow the Lab or Venue standard sanitation operating procedures for routine cleaning and disinfecting. Considering COVID 19, however, you may need to create or enhance existing protocols.
In addition to scheduled cleaning, disinfecting, and sanitizing, the demand for immediate cleaning will also present. Clean surfaces and objects that are visibly soiled. If surfaces or objects are soiled with body fluids or blood, use gloves and other standard precautions to avoid coming into contact with the fluid. While wearing gloves remove the spill, and then clean and disinfect the surface, and then clean and disinfect your hands.
Clean and disinfect correctly
One of the most effective things that you can do to increase the effectiveness of the venue’s standard sanitation operating procedures is to follow the product directions.
Wash surfaces with a general household cleaner to remove germs. Rinse with water and follow with an EPA-registered disinfectant to kill germs. (My source here is the US CDC. Please contact your country’s infectious disease authority to see if they have a list of tested and approved products if the products on the CDC’s list are not available in your area.)
If a surface is not visibly dirty, you can clean it with an EPA-registered product that both cleans (removes germs) and disinfects (kills germs) instead. Be sure to read the label directions carefully, as there may be a separate procedure for using the product as a cleaner as compared to using it as a disinfectant. Disinfection usually requires the product to remain on the surface for a certain period of time.
EPA Press Release Disinfectants to use against COVID 19
Disinfectants for Use Against SARS-CoV-2 (COVID-19)
Use products safely
Please use products safely. Bleach is good. Ammonia is good. Bleach + ammonia is not twice as good. As a matter of chemistry, it can be lethal. Please read labels.
Do not mix cleaners and disinfectants to make your own Super-Cleaner unless the labels explicitly indicate that it is safe to do so. Combining certain products can result in serious injury or death.
Pay close attention to hazard warnings and directions on product labels. Cleaning products and disinfectants often call for the use of gloves or eye protection. For example, gloves should always be worn to protect your hands when working with bleach solutions.
Ensure that venue staff, instructors and others who use cleaners and disinfectants read and understand all instruction labels and understand safe and appropriate use. This might require that instructional materials and training be provided in other languages multiple languages or infographics.
Regarding bleach, check the label to see if the bleach is intended for disinfection and has a sodium hypochlorite concentration of 5%–6%. Ensure the product is not past its expiration date. Some bleaches, such as those designed for safe use on colored clothing or for whitening, may not be suitable for disinfection. Here is an acceptable cleaning and disinfecting bleach recipe, assuming the previously stated conditions.
- 4 teaspoons bleach per 1 quart of room temperature water
- 20 milliliters bleach per 1 liter of room temperature water
- Label the container BLEACH DISINFECTING SOLUTION
This bleach solutions would be effective for disinfection for up to 24 hours.
Regarding alcohol, the use of solutions with at least 70% alcohol are considered effective.
Handle waste properly
The most effective way to maintain your cleaning, disinfecting, and sanitizing is to properly handle and dispose of the waste materials.
Follow your venue’s standard procedures for handling waste, which may include wearing gloves. Place no-touch waste baskets where they are easy to use. Throw disposable items used to clean surfaces and items in the trash immediately after use. Avoid touching used tissues and other waste when emptying waste baskets. Wash your hands with soap and water after emptying waste baskets and touching used tissues and similar waste.
Personal practices
Ultimately, the most effective way to deal with COVID 19 is to not spread COVID 19.
Please see the Personal Practices Infographic thumbnail menu on the next page. The menu includes links to free downloads. At a minimum, best practices would have the 3 that are available in 27+ language versions printed in the appropriate languages and displayed in the lab or venue.
As an oversimplification: fewer people is better than more people, further apart is better than closer together, a mask covering mouth and nose is better than a mask covering mouth only or no mask at all, fresh air is better than recirculated air, outside is better than inside.
Other personal practice considerations would be for the lab or venue to encourage the use of PPE Personal Protective Equipment and supplies. Better still, for the lab or venue to provide PPE. Best practices PPE and supplies may include but not be limited to the following. Hand sanitizer solution of 70% or more alcohol placed at the entrance and exits of rooms and the building, gloves, face masks, face shields foot peddle opening garbage can lids and foot assisted door opening and closing mechanisms or attachments.
The goal is not to eliminate risk, that is not realistic. The goal is to reduce the overall risk by eliminating the risk associated with the seven concept areas above. If you can remove a few of the individual items, then you have reduced the overall risk. The more items reduced or removed, the lower the overall risk and the higher the level of safety.
|
The links (below graphics) go to the source of the infographics. Many are available in multiple languages. |
||
|
|
||
One of the most effective things that you can do to reduce the risk of spreading a virus or bacteria and lower the number of germs in a venue or lab is to sanitize the High-Touch Points.
We have created a High-Touch Point checklist that is representative, but not exhaustive, for identifying commonly touched places in a venue or lab. We suggest that you use this checklist as a guide and walk through the venue thoughtfully considering what you touch. What an attendee might likely touch often. What might logically be touched by multiple attendees. As an exercise, stand outside of your lab or venue and then slowly enter and move through the facility noting the things that you do touch and the things an attendee would touch. Please use this list as a general guide.
- Entering the venue
- The outside door handle plus a 1-foot radius of the door surrounding the handle
- The inside edge of the open door above the latch
- The inside door handle plus a 1-foot radius of the door surrounding the handle
- The light switches plus a 6-inch radius of the wall surrounding the switch plate
- The thermostat
- The alarm panel
- The desktop telephones and computer workstations
- Is there the means to wash or use 70% alcohol hand sanitizer upon entry?
- Is the door easily adapted to no touch / low touch opening and closing?
- Is it possible to have a tissue box by the door so the attendee can use the tissue as a barrier between their hand and the doorknob? And if so, is there a trash can located in the door area for its disposal?
- Entering the classroom
- The doorknob / handle
- The light switches
- The tops and backs of the chairs
- The table / desk surface
- The course provided notebook / workbook
- The instructor workstation / lectern
- The audio-visual remote controls
- Is there the means to wash or use 70% alcohol hand sanitizer upon entry?
- Is the door easily adapted to no touch / low touch opening and closing?
- Is there a cleaning and disinfecting mechanism like wipes, a spray bottle with bleach solution and paper towels readily and visually accessible?
- Hospitality
- The coffee cup counter area
- The coffeepot / airpot / coffee service vessels
- The water fountain / dispenser / pitchers
- The snack counter and containers. Individually wrapped snacks and baked goods are more hygienic than open and unwrapped snacks and baked goods.
- The refrigerator handle and door
- The plates and cutlery containers. Paper plates and wrapped cutlery is more hygienic than open plastic or metal cutlery and plastic or ceramic plates.
- Is there a cleaning and disinfecting mechanism like wipes, a spray bottle with bleach solution and paper towels readily and visually accessible?
- Are napkins or gloves visibly available?
- Is a garbage can in the immediate area?
- Are snacks, food items and cutlery individually wrapped?
- Internal doors and walls
- The door handles on both sides of the door plus a 1-foot radius of the door surface surrounding the handle
- The inside edge of the door above the latch
- The light switch plus a 6-inch radius of the wall surrounding the switch plate
- The plug receptacle plus a 6-inch radius of the wall surrounding the plug plate where USB charges and laptops have been plugged in by attendees
- The light switches plus a 6-inch radius of the wall surrounding the switch plate
- Light switches, receptacles and surge protectors are often overlooked.
- Can doors be made to not latch so a person’s foot can upon or close it?
- Entering the cupping room
- The door handles on both sides of the door plus a 1-foot radius of the door surface surrounding the handle and the inside edge of the door above the latch
- The light switch plus a 6-inch radius of the wall surrounding the switch plate
- The cupping tabletops and edges
- The hot water tower spigot handles and machine face and the click kettles, glass carafes and other hot water vessels
- The cabinet doors and drawers
- The grinders, brewers and airpots
- The cupping room accessories like timers, scales, calculators, clipboards, etc
- The sink, faucet, and water tap handles
- The garbage cans, lids, and sludge buckets
- Can doors be made to not latched so the attendee can open or close it with their foot?
- Are cleaning and disinfecting materials and paper towels readily visible and in sufficient supple?
- It may take 15 mins or more to disinfect a cupping room with 1 person per table working. 2 staff 2 tables = 15 +/-. 1 Staff 2 tables = 30 +/-.
- Restrooms
- The toilet tank lid, seat, and flusher handle
- The sink, faucet and water tap handles
- The grab / assist bars
- The wall and a 1-foot radius of the wall around toilet paper area.
- The bidet hose handle
- Any surface within arm’s reach of a seated position on the toilet
- The soap and paper towel dispensers
- Door handles on both sides of the door plus a 1-foot radius of the door surface surrounding the handles and the inside edge of the door
- The light switch plus a 6-inch radius of the wall surrounding the switch plate
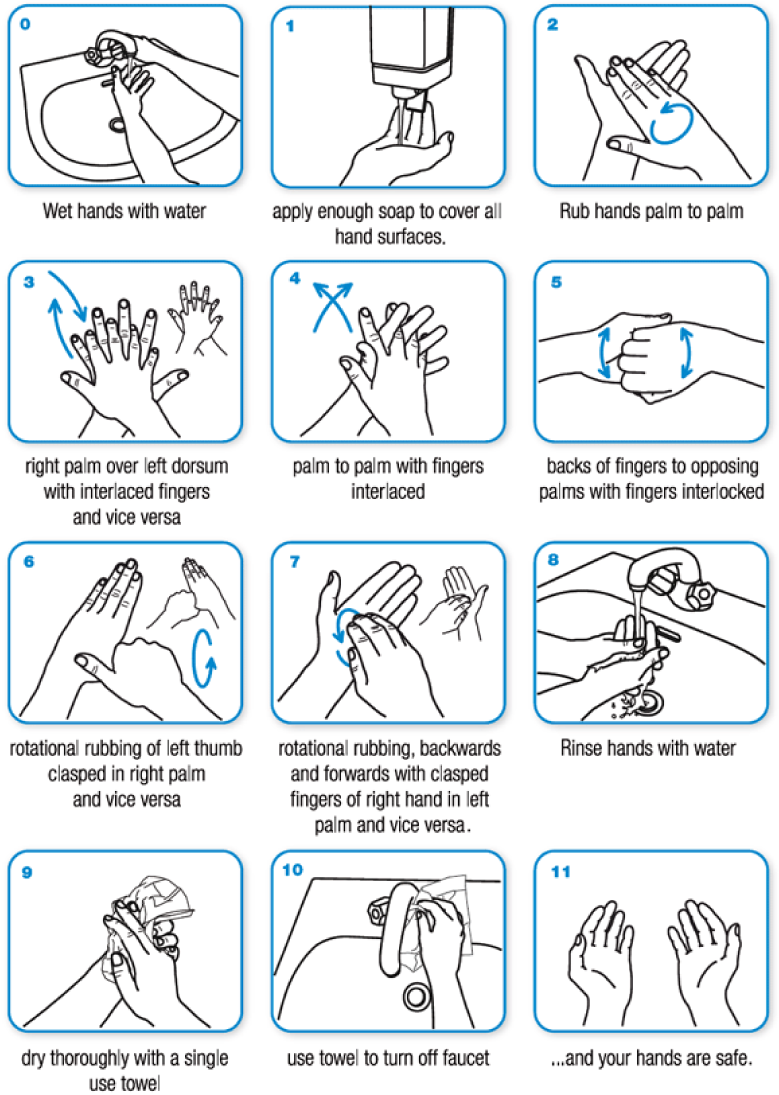
- Is there signage in the restroom detailing how to thoroughly wash hands?
- Is the garbage can next to the door so that the user can use paper towels to open the door and then dispose of the paper?
- Does the trash can have a no touch lid?
